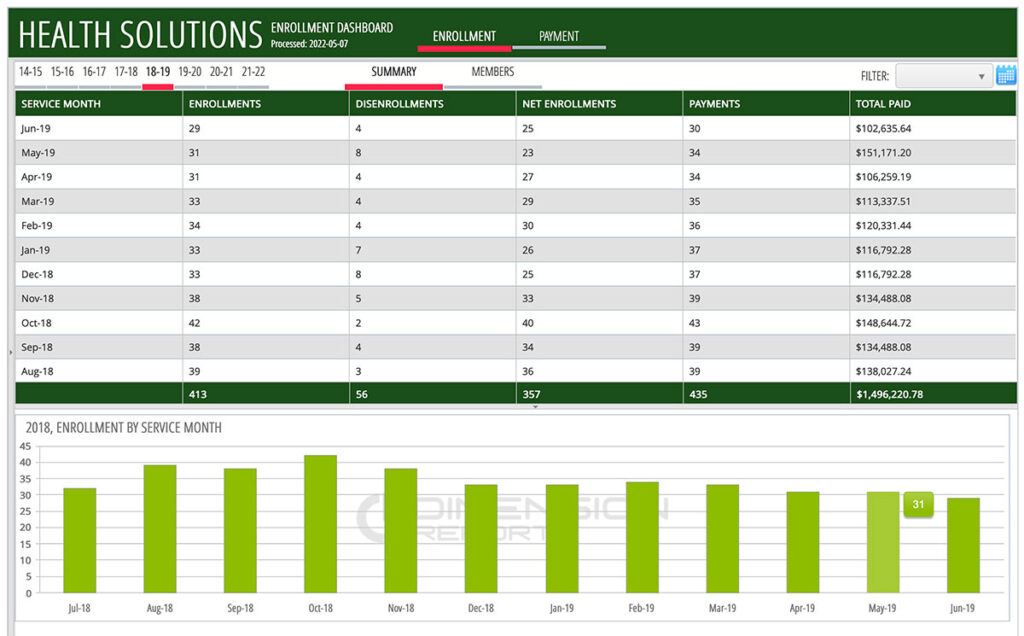
Enrollment Reporting
Dimension Reports DR-Enrollment provides automated reporting for Managed Care Enrollment, providing a solution for the complex task of reconciling enrollments with capitation payments and tracking enrollment, disenrollment, beneficiaries and rates.
Payment Reconciliation
By tracking enrollment payments, verification that enrollment periods are paid is easy (screen capture).
Enrollment Status Tracking
Track historical enrollment status and view retroactive changes going back two years (screen capture).
Beneficiary Details
With a clear, interactive and visual interface, tracking attributes of beneficiaries can allow for anticipated rate changes and help resolve missing or insufficient payment based on factors such as changes in aid code or demographic category (screen capture).
Rapid Deployments
Using existing 834 and 820 HIPAA Transactions and deploying Software-as-a-Service, the report solution can be ready for use within a matter of weeks.
Features
Fiscal Year Breakdown
Data is organized by service or payment years allowing analytical versatility (screen capture).
Enrolled/Disenrolled Tracking
Enrollment has status of enrolled or disenrolled (screen capture).
Remittance information
Identify enrollment and paid amounts tied to individual warrants (screen capture).